Carpal Tunnel Syndrome
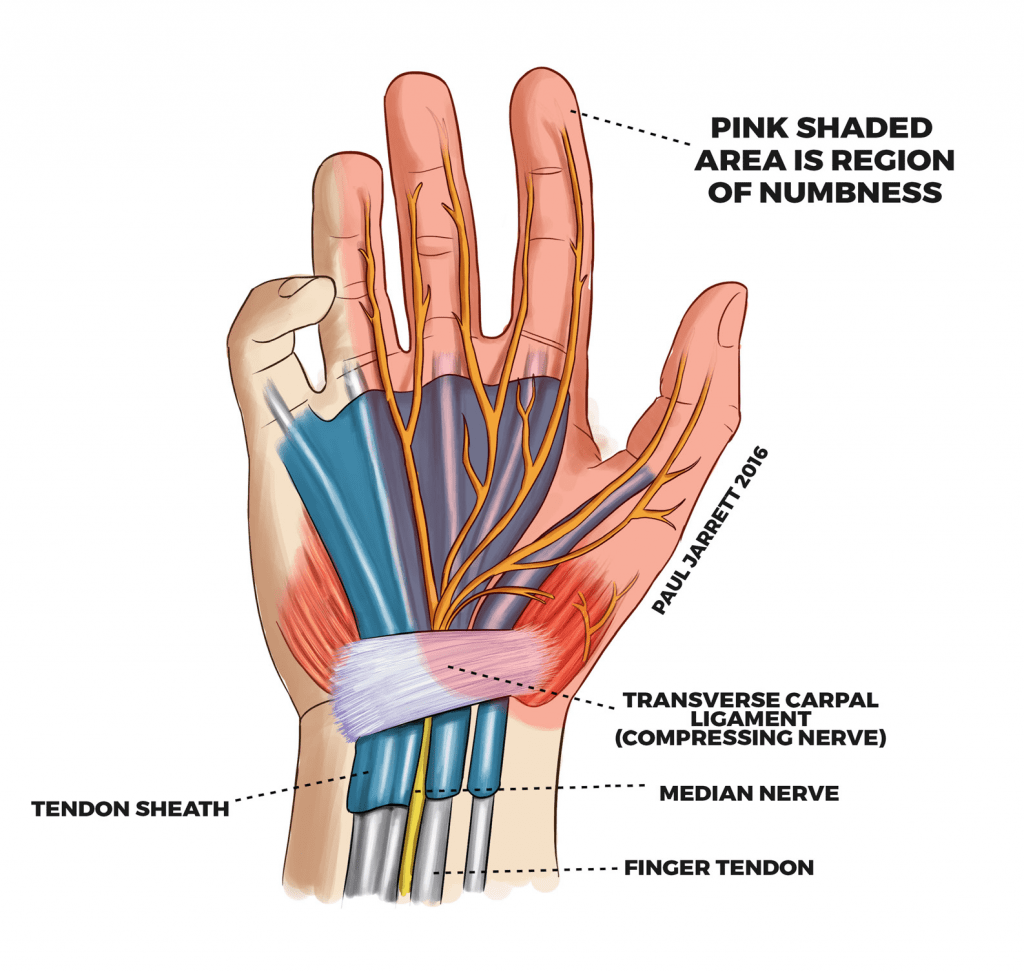
The median nerve, a large nerve supplying some of your hand’s function, enters the hand from your forearm by passing through a tunnel bound on the back of your wrist by several bones, and on the palm side of your wrist by a thick ligament called the transverse carpal ligament. This tunnel is called the Carpal Tunnel.
If the nerve becomes compressed within the tunnel, it fails to function normally and the symptoms of Carpel Tunnel Syndrome result. It is possible for conditions which cause swelling of the body, or for lumps such a ganglion (fluid filled cysts) to result in compression of the median nerve, but the usual cause for Carpel Tunnel Syndrome is called “idiopathic carpal tunnel syndrome” the cause of which is not fully understood.
CTS is a common hand disorder; approximately 1 in 10 people in Australia have surgery for this condition during their lifetime. It is especially common in late pregnancy, following childbirth, and is more common in individuals with medical conditions including diabetes or thyroid disease.
A person with carpal tunnel syndrome would usually experience pins and needles and numbness in the thumb, index, middle, ring and often the little finger, in addition to pain in the wrist sometimes going up into the forearm. If you have numbness in the little finger, this is due to compression of a different nerve called the ulnar nerve, often at the wrist or the elbow.
CTS can develop over a short period, or often over a period of some months or years. The affected hand may feel weaker than normal and clumsy. Sufferers often drop items or find it difficult to manipulate small items. The symptoms can cause insomnia and can be quite debilitating if severe. CTS can occur in both hands at the same time.
A specialist orthopaedic surgeon (read about Dr Jarrett) should assess you and your hand to confirm the diagnosis, ensure there are no additional conditions present to cause the symptoms and to investigate any particular causes for the Carpel Tunnel Syndrome.
Sometimes an additional nerve test called Nerve Conduction, or EMG Studies can be useful to confirm the diagnosis and ascertain how poorly the nerve is working. Your doctor may also arrange an ultrasound to help establish whether you have Carpal Tunnel Syndrome.
Nerve conduction studies are carried out by a Neurologist who passes small electric currents within your arm and hands to measure the way that the electrical signals travel along the nerves. It is not necessary for every patient with CTS to have nerve conduction studies before having treatment.
About Carpal Tunnel Syndrome
In this video Dr Paul Jarrett explains what Carpal Tunnel Syndrome is, how it can affect your hand, wrist and forearm, and what treatments are available to stop Carpal Tunnel Syndrome.
How is carpal tunnel syndrome treated?
Did you know?
Dr Paul Jarrett performs over 200 Carpal Tunnel operations every year!
Should non-operative treatment be unsuccessful, an operation called a Carpal Tunnel Decompression (CTD) is usually recommended. CTD is by far the most reliable treatment for CTS.
If longstanding CTS has scarred the nerve, it is possible that recovery may be limited.
Endoscopic Carpal Tunnel Decompression An alternative to making a small wound in the palm is to make a small wound at the wrist and undertake the operation using an endoscope (telescope). The endoscopic carpal tunnel decompression has a slightly quicker recovery, but statistically, has slightly higher risks.
Dr Jarrett commonly performs the operation through the small wound in the palm but can undertake the procedure endoscopically if you would prefer this.
Ready to remedy your carpal tunnel syndrome?
Use this form to send us your referral letter and we’ll call you back to arrange an appointment. Dr Jarrett will assess your condition and advise on the best treatment option for you. If you have any questions / concerns, please call us on 1300 527 738.After your operation.
In this video, our Orthopaedic Nurse, Emma, explains how to care for and dress your wound after Carpal Tunnel Surgery.