Shoulder Arthritis
The glenohumeral joint may, either as a result of previous injury, inflammatory diseases or genetic reasons, develop arthritis.
This, to a greater or lesser degree, will cause shoulder discomfort or pain, stiffness and reduced shoulder function and often represents a considerable problem to your life.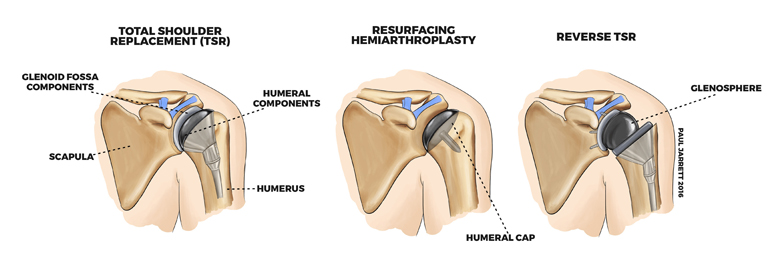
How is arthritis of the shoulder treated?
Non-Operative
Operative
Non-Operative
If your symptoms are mild, then no treatment or an occasional pain-killing medication is usually the best way of proceeding.
If your symptoms are troublesome then physiotherapy is the best place to start, and may be sufficient to improve matters. If not, some patients may benefit from a steroid (cortisone) injection, although these injections are not reliable and often their assistance is temporary.
Operative
If your symptoms are severe, the conventional treatment is shoulder replacement surgery, of which we have a number of types:
Hemiarthroplasty surfacing replacement re-covers the damaged humeral head (ball of the joint) with a metal implant.
Total shoulder replacement replaces the entire ball and also the socket of the joint.
Reverse total shoulder replacement is a treatment for arthritis associated with significant rotator cuff tears or some shoulder fractures, places a new ball on the original socket and a socket in the original ball.
A shoulder replacement requires a general anaesthetic. A moderate sized incision is placed on the front of your shoulder with one tendon being partially detached to access your joint. The replacement is inserted, and the soft tissue including your tendon is repaired.
The risks of shoulder replacement include the risks of shoulder surgery mentioned later in this booklet, but also include dislocation and/ or failure of the implant. If the joint dislocates, it may require a general anaesthetic to re-locate by manipulation, or in some instances, the replacement implants will need to be changed. A shoulder replacement is like anything man-made, capable of wearing out in your lifetime, and occasionally the implant may wear out earlier than expected or may stop working e and require revision replacement.
Revision replacement in the shoulder is complex, as there is a relatively little bone to work with compared to a joint like a hip, and revision replacements do not usually function as well as the initial implant. At times there can be insufficient bone to revise the implant which will result in very poor shoulder function and symptoms. Due to these risks, it is imperative to make sure a shoulder replacement is the right operation for you, and the decision-making process will involve an extensive discussion with Mr Jarrett.
Shoulder Replacement Post-Operative Care
At least one night in hospital is required, and a sling is worn in the initial stages, but exercises commence the day following your operation. Your sutures will all be beneath your skin and dressings can be removed 10 days following surgery (please see our website for a video regarding dressings removal). You will require physiotherapy following your shoulder replacement and Mr Jarrett will arrange a physiotherapist consultation before surgery to go over your exercises pre-operatively. It often takes over a year to maximally improve following a shoulder replacement, with the bulk of the improvement in the first 3-6 months.