Cubital Tunnel Syndrome
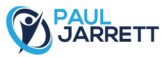
The ulnar nerve as it travels through the lower part of the arm, the elbow and into the top part of the forearm runs through several areas in which it can be compressed or stretched. This compression may occur without an apparent cause, but can also be due to prominent areas of bone at the elbow from arthritis, or from injury or a ganglion (bubble of fluid) from the joint. If the nerve is compressed it can stop working properly which causes symptoms of pins and needles and numbness in the little finger, and the ring finger side of the hand, with pain often on the inner aspect of the elbow, which can travel towards your hand.
Some people will feel that their hand is less strong or less dexterous. The symptoms are a bit like when you hit your “funny bone” (the “funny bone” is, in fact, your ulnar nerve). The medical term for problems with the ulnar nerve at your elbow is ulnar neuropathy or cubital tunnel syndrome. The symptoms often occur at night, and when bending the elbow for prolonged periods.
How is cubital tunnel syndrome treated?
Milder cases of cubital tunnel syndrome may cause relatively little symptoms or only occur occasionally during prolonged activities (for instance, when Mr Jarrett typed this section he had been on a plane typing in a cramped position for 6 hours, and had mild tingling in his little and ring finger on one side). However, treatment is useful for more significant symptoms, and either takes the form of wearing a splint at night, undertaking exercises to assist the ulnar nerve to glide better at the elbow, or one of a number of operations detailed underneath.
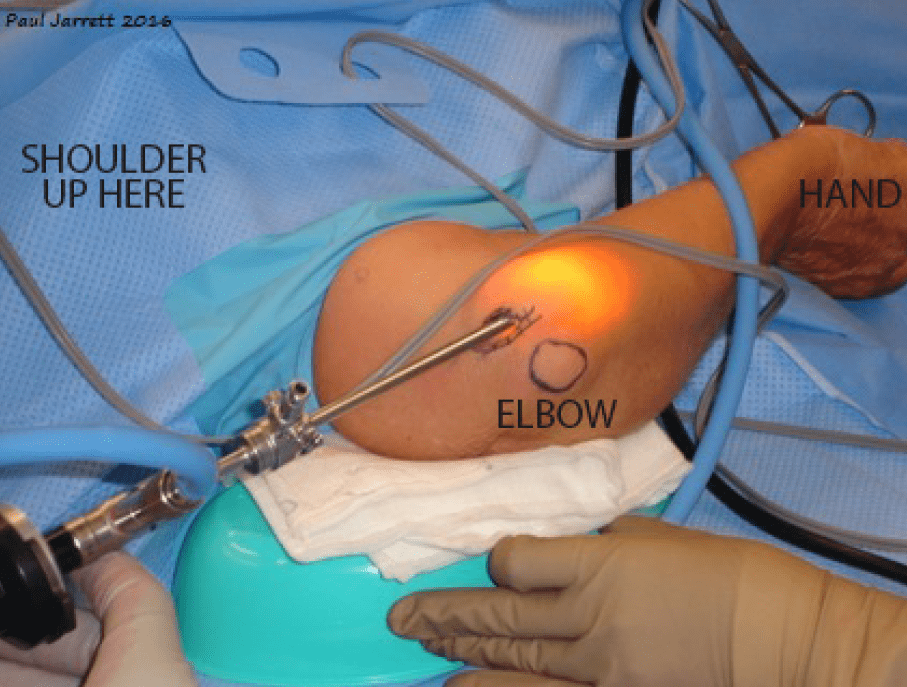
The nerve can be surgically decompressed by releasing the overlying structures causing compression. This can be undertaken via a medium length wound on the inside of your elbow under direct vision (open ulnar nerve decompression), or most commonly via an approximately 2 cm wound using a telescope (endoscopic ulnar nerve decompression).
At times the nerve is best moved from its original position into a position slightly in front of your medial epicondyle and this version of the operation is called anterior transposition. This is at times necessary if the nerve is unstable at the end of decompressing it or if the nerve looks stretched in its original position and by moving its position the tension on it would be reduced.
For ulnar nerve surgery, most patients find that they improve by at least 75% and most people are left with some mild symptoms in the long term. In particular, if the cubital tunnel syndrome was very long standing or severe, recovery of sensation will be less as the nerve may have been damaged by being compressed for a long period.
An ulnar nerve transposition is a bigger operation than the decompression of the nerve and takes a longer time to recover with slightly higher risks. For some patients, this is the most appropriate operation, but for the many, a decompression is the best choice.
Cubital Tunnel Syndrome –
Post-Operative Care
The above operations are usually carried out under general anaesthetic. The decompression is often a day case, and occasionally transposition procedures may require a night stay in hospital.
A large bandage will be in place for the first two days post-surgery, and then a sticky plaster until 10 days after the operation. Generally, no suture removal is required. The motion of your elbow can be commenced immediately after your operation, and movement does return faster after decompression, especially if performed endoscopically.
There will be some bruising in the forearm after the operation, and the numbness will probably not disappear immediately. You can expect to return to work in 2-7 days for light activities, and 1-6 weeks for full activities after an endoscopic decompression.
For transposition, light duties are often possible by two weeks and heavier duties between 6-12 weeks. One important risk, especially for the open decompression and transposition, is long-term numbness in an area of skin at the back of the forearm due to stretching, or less commonly, injury to the skin nerves to the area.
There is also a risk of damage to the ulnar nerve at surgery.